Admission Line (866) 396-3655
Minority Mental Health & Substance Abuse & The Barrier to Finding Care
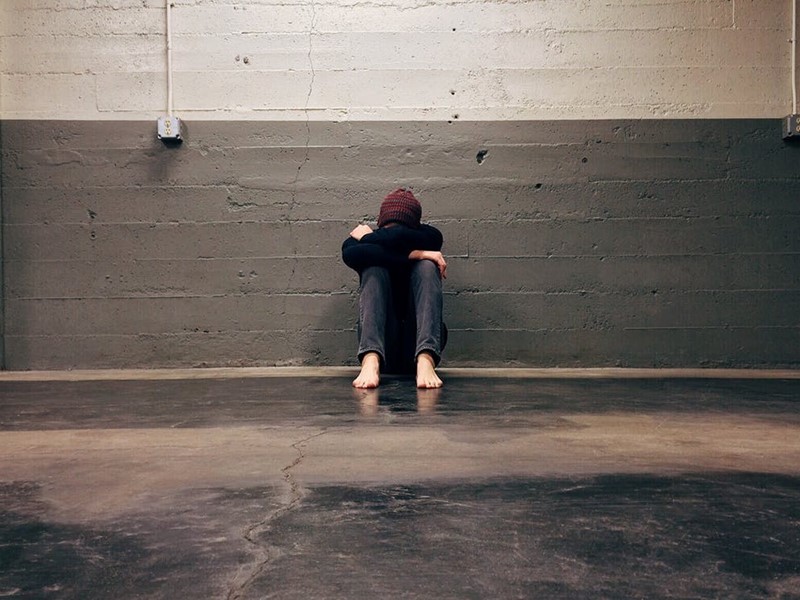
Accessing mental healthcare is difficult or impossible for a significant number of people. More than half of the adults in the U.S. who experience mental illness do not receive treatment.
The barriers that prevent access to mental healthcare disproportionately affect minorities. People of color, low-income households, and LGBTQ+ individuals often go without the treatment they need.
The same is true of substance abuse and recovery. People in minority groups often struggle to find affordable, compassionate, culturally-informed care.
Understanding and acknowledging these barriers was a crucial first step. Now, mental healthcare professionals and advocates seek to dismantle them. Their goal is to provide everyone with adequate care.
Top 6 Barriers to Accessing Mental Health Care
Several obstacles may stand in the way of accessing care. Some are inherent qualities, while others are external factors.
A person may experience one or more of these barriers in their lifetime. Each additional risk factor increases the likelihood that they won’t find the treatment they need.
1. Financial Barriers
The cost of treatment is often prohibitive. Thanks to the Affordable Care Act, insurance carriers are required to cover mental health treatment. Even so, the price after insurance may still not be viable for many households. A family may be forced to prioritize other expenses over the cost of treatment.
A lack of health insurance can also put treatment outside the realm of possibility. A person who can’t afford insurance or is unemployed has little recourse. Not every job offers health insurance benefits.
Without insurance, the cost of a traditional talk therapy session ranges from $65 to $250. Those with chronic issues, such as substance abuse, will need more than a single session. Getting more intensive care costs even more.
2. Racial and Ethnic Barriers
People who belong to a racial, ethnic, or cultural minority group are more likely to struggle to access care than white people. The reasons for this include:
- Financial disparities
- Lack of diverse representation among mental health professionals
- Cultural attitudes
- Language barriers
- Implicit bias and racism
People of color are also more likely to experience other hardships that put them at a disadvantage. 27% of Black Americans live below the poverty level, as opposed to 10% of white people.
A shortage of diverse providers is a significant problem. People of color, in general, are less likely to find a provider from the same minority group. The American Psychology Association (APA) found that 84% of U.S. psychologists are White. Connecting with a provider with whom you feel safe and understood is an essential ingredient in mental healthcare.
3. Social Stigma
There has long been a stigma attached to mental illness and receiving care for it. While this stigma is slowly dissolving, it still exists in many circles. Living in an area or situation where the stigma is prevalent can be a significant barrier.
Asking for help around mental illness or substance abuse may be impossible for some people. Even the act of admitting it can be a challenge. They may struggle to confront it internally or fear the reaction they would earn from their family or social circles. They might worry that people would treat them differently or that there would be consequences at work.
Eradicating the stigma and shame around mental illness is critical for increasing access to care.
4. Education and Awareness
Mental illness has long flown under the radar, especially compared to physical disease or injury. It is often considered “invisible” because you can’t immediately recognize it in a person from looking at them. It can also be challenging to diagnose and understand.
Society's attitudes have often misrepresented people with different mental illnesses as being lazy, dramatic and emotional, or worrying too much. Only recently has mental illness come into sharper understanding in the broader culture.
Organizations like the National Alliance on Mental Illness (NAMI) are hard at work increasing awareness around mental illness, educating the public about it, and destigmatizing it in its many forms.
5. Shortage of Mental Health Professionals
The U.S. is facing a general shortage of medical professionals, especially in mental healthcare. The Health Resources and Service Administration (HRSA) reports that 149 million Americans live in an area with insufficient mental healthcare providers to serve the local population.
Even fewer mental health professionals offer services for lower-income clients or those without insurance. Those who do are often flooded with demand and may experience long waitlists to make an appointment.
6. LGBTQ+ Barriers
Individuals in the LGBTQ+ community are 2.5 times more likely to experience depression, anxiety, and substance abuse than cisgender heterosexual individuals. They face more challenges relating to their identity, often from people close to them.
Some do not feel safe revealing their identity, which can interfere with accessing care that addresses their needs. The lack of acceptance from friends and family can also increase the prevalence of suicidal thoughts.
Barriers to Preventing and Treating Substance Abuse
Substance abuse has a few more barriers that can prevent people from getting the help they need. These barriers include:
- A complicated system—Because substance abuse treatment requires coordination of so many different providers and disciplines, it can be confusing to navigate.
- Insufficient hospital capacity—Substance abuse treatment can sometimes involve hospitalization. Inadequate hospital capacity can prevent everyone from receiving treatment, especially in rural areas.
- Lack of motivation for change—Not everyone is ready to receive treatment. Programs must address patients’ motivation for change, or lack thereof, before treatment can succeed.
A high level of communication, coordination, and compassion is necessary for substance abuse treatment to be accessed, much less successful.
How to Improve Access to Mental Health Care
Though these barriers are real and challenging for many people today, there are also reasons to feel hopeful.
Mental health and substance abuse have entered more conversations than ever. Advocates, mental health professionals, and researchers are all busy uncovering ways to improve mental health care access for everyone.
More Awareness, Less Stigma
Creating awareness and developing more education around mental health care are the first steps to breaking down these barriers. Part of this process is removing the stigma that still surrounds mental illness.
Defanging stigma is a team effort. Medical providers, therapists, religious leaders, teachers, and community organizers must receive education on how stigma clouds mental health care. The misconceptions around mental health must be clarified. Support from family, friends, and community must be emphasized.
Talking openly about what you’ve been through without shame can act as an example to others. If you feel safe doing so, sharing your experience is one way to contribute to increased awareness and decreased stigma around mental health.
Culturally Appropriate Care
Efforts to train and hire more mental health professionals from diverse backgrounds are another essential piece of the puzzle. Many people feel safer or more comfortable opening up to someone who shares or relates to their experience.
The good news is that more people from minority groups than ever are matriculating into psychology programs. That means more diverse providers for more patients. Until that happens, culturally appropriate training must be offered to all mental health professionals so they can confidently treat their patients.
Asking the Right Questions
Mental health care needs to become a permanent part of primary care. Primary care providers need to conduct mental health screenings in their offices. Screenings can help reveal mental illness that has gone underlooked. It can also help patients to become more self-aware and attentive to what they’re experiencing.
Communication is the most important element of mental health care. Treatment for any mental illness or substance abuse issue requires clear communication and understanding. Providers must learn how to ask the right questions and how to truly hear what their patients say.
Get the Care You Need
If you’re struggling with mental illness or substance abuse, you deserve treatment that will help you live a full and healthy life. There is no shame in experiencing these issues, and mental health professionals are here to help.
Whatever you’re dealing with, treatment is out there. Jackson House can help you access the care you need. Explore your treatment options today.
